The NHS is currently facing a critical challenge with its ageing digital infrastructure. Attempts to implement a centralised patient record system, which would enable access to patient data across all NHS locations, have been fraught with difficulties.
The NHS is currently facing a critical challenge with its ageing digital infrastructure. Attempts to implement a centralised patient record system, which would enable access to patient data across all NHS locations, have been fraught with difficulties.
A number of issues contribute to this problem: incompatible IT systems that cannot communicate with each other, outdated infrastructure, delayed correspondence due to inefficient systems, inconsistent IT setups across locations, continued reliance on paper records, and the need for multiple logins by staff.
Some aspects of the issue are relatively straightforward to address. For instance, upgrading to modern IT systems and phasing out unsupported platforms, such as those running obsolete versions of Windows, can be achieved with sufficient investment and planning.
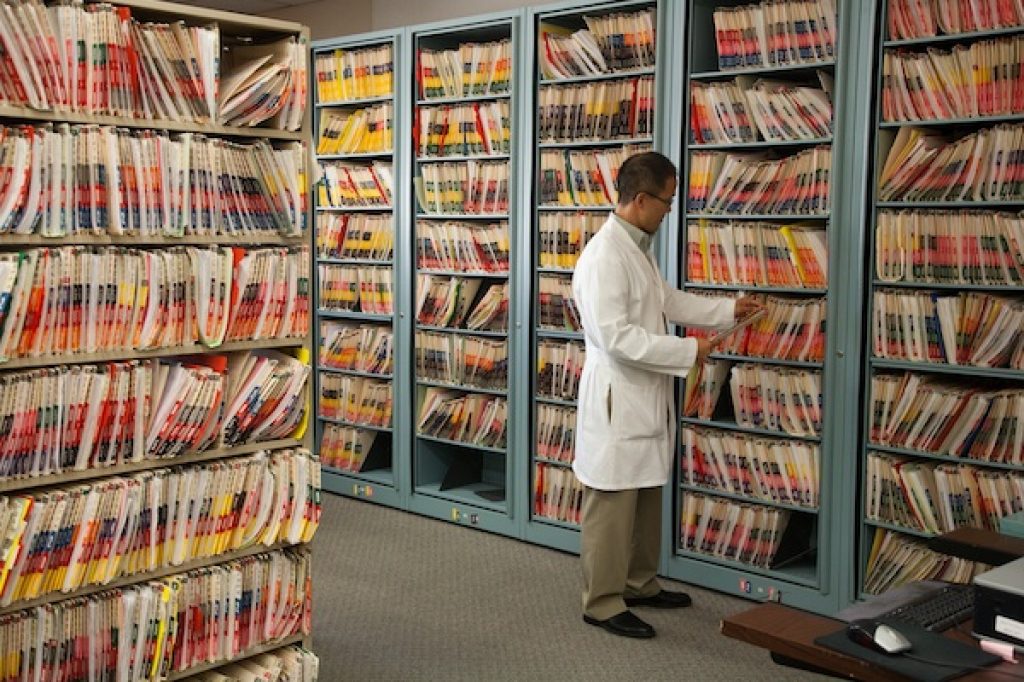
Other challenges are more complex. Reliance on paper records is a significant obstacle. As of recent reports, 4% of NHS trusts rely entirely on paper records, while 75% use a hybrid of paper and digital systems. Digitising paper records, whether manually or through AI, is a time-consuming task and demands a high degree of accuracy.
This raises some important questions:
- How would a new digital system be implemented?
- Would it replace all existing systems entirely?
- How would patient data be migrated?
One proposed solution is to register only patients born after the new system’s introduction on the updated platform. However, this poses its own dilemma: should existing patients be migrated, with the associated risks of data errors, especially from paper-based records, or should their information remain on legacy systems, effectively requiring parallel systems to operate for decades?

Newer technologies offer promising capabilities, such as compatibility with modern software upgrades. In one case, a simple software driver update resulted in a 16% improvement in processing speed.
However, even the most advanced system will falter without proper staff training and engagement. If staff are unable or unwilling to adopt new systems effectively, then progress will be severely hampered. Furthermore, improper use of the system, such as mislabelled drop-down options or poorly structured free-text entries, can severely compromise data quality and any resulting analysis.
As such, buy-in from the leadership is crucial. NHS leaders must champion the use of new systems and ensure correct usage. This enables high-quality data collection, which can then be used for real-time analytics and automated dashboards. Without such buy-in, there is a risk of staff reverting to unofficial workarounds, undermining the new system.

Despite the challenges, there are some bright spots. Some NHS services have successfully adopted innovations, such as automated bed management systems that track real-time availability, and image recognition technologies aiding in cancer diagnoses and blood cell analysis. These examples offer a glimpse of what is possible when digital transformation is embraced.